Tepezza
Upon the cell surface of the apical microvilli of the thyroid acini is expressed the thyroid microsomal antigen. The thyroid acini are polarized and may be intact or semi-intact.
By understanding this structure, it is possible to visualise how common antibodies that are associated with thyroid autoimmune disease lead to complement mediated and antibody dependent cell toxicity.
Based on research studies, TSH receptor antibodies are now classified into two types. The first includes those that stimulate thyroid hormone synthesis and release (called TSI), while the second is one that mimics the role of TSH in its growth promotion role (called TGI).
In patients who have goitrous Grave’s disease and in a few with euthyroid non-toxic goitre, the presence of TGI has now identified novel thyroid autoimmunity.
In a majority with nontoxic goitre, there is a specific lack of lymphoid thyroiditis and a reduced chance of occurrence of thyroglobulin or microsomal antibodies. Instead, the autoimmunity is expressed through hyperplasia and hypertrophy of the thyroid gland itself.
While both TSI and TGI have stimulating effects, they can also have blocking effects and have been called TSI block and TGI block respectively.
In myxoedema, the thyroid gland atrophy occurs due to impaired pituitary controlled repair. This is because of high prevalence of these blocking antibodies.
However, in goitrous thyroiditis, these blocking antibodies do not exist. This leads to uninhibited TSH influence on the thyroid gland.
The presence of these antibodies can be easily confirmed in euthyroid subjects. Those who receive TSI blockers do not develop hyperthyroidism, while those who receive growth promoting antibodies eventually develop a goitre
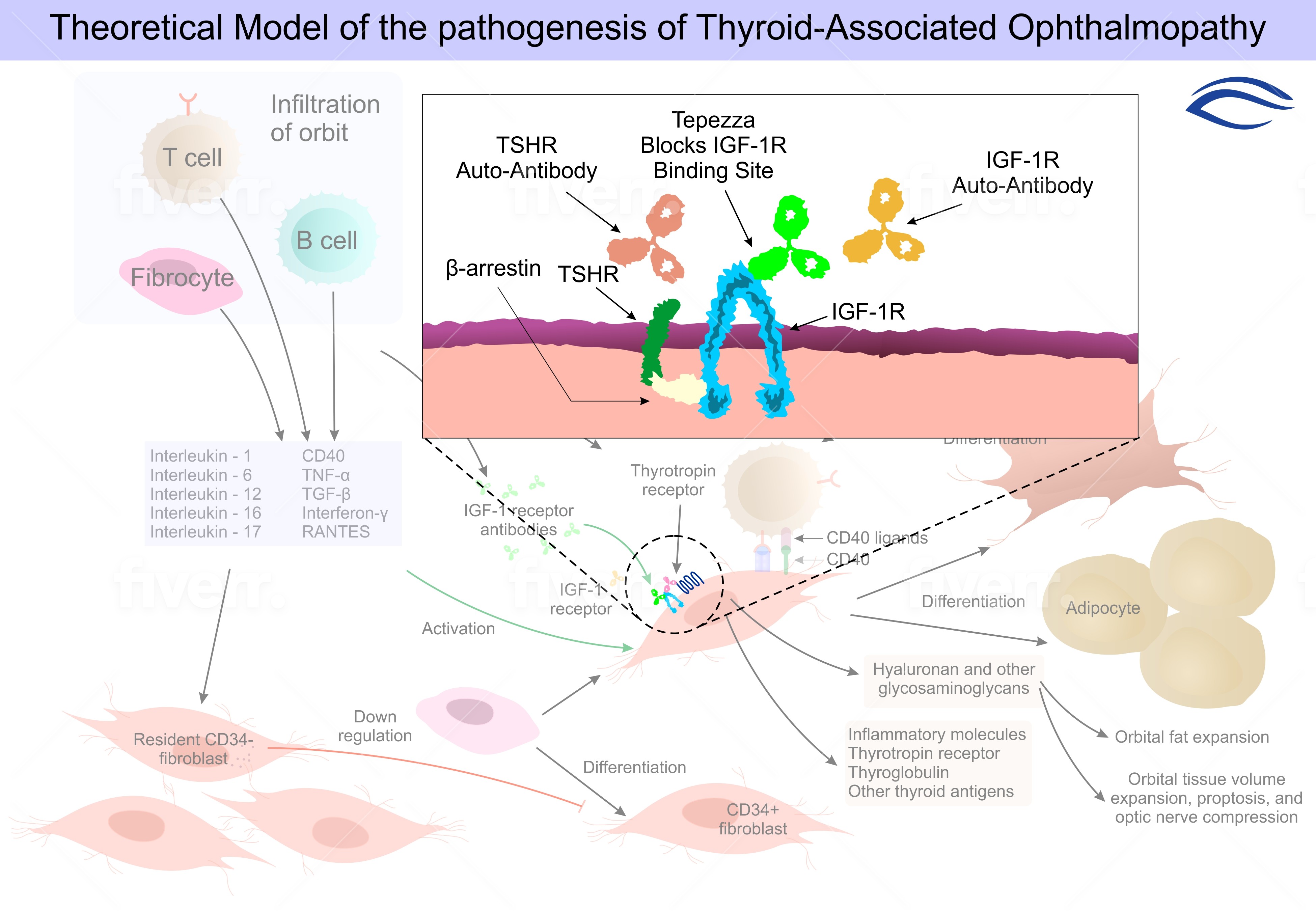
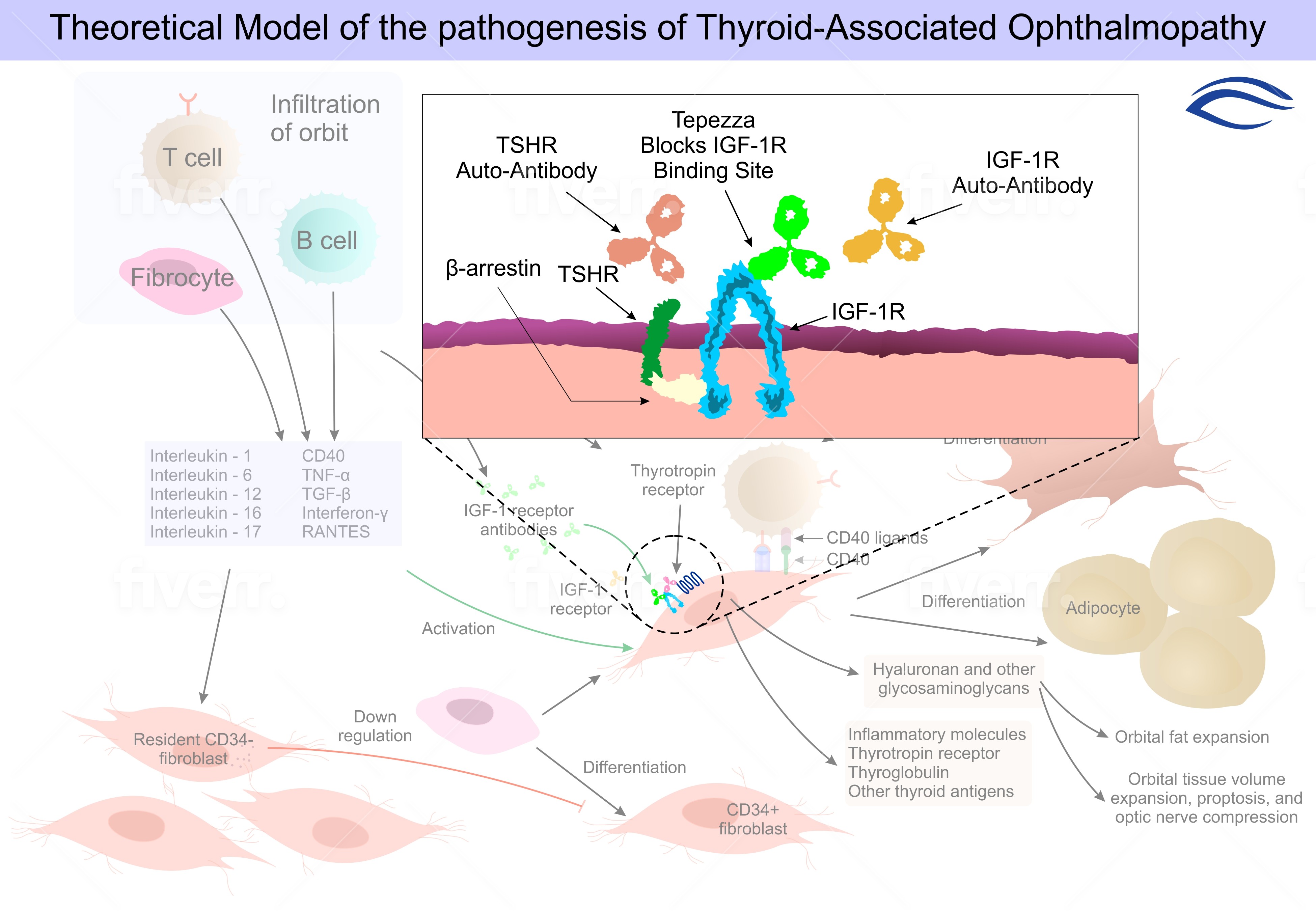
Thyroid-associated ophthalmopathy, a condition commonly associated with Graves’
disease, remains inadequately treated. Current medical therapies, which primarily
consist of glucocorticoids, have limited efficacy and present safety concerns. Inhibition
of the insulin-like growth factor I receptor (IGF-IR) is a new therapeutic
strategy to attenuate the underlying autoimmune pathogenesis of ophthalmopathy
Current treatments are inconsistently beneficial and often associated with side effects,
- Previous clinical trials suggest that high dose glucocorticoids, alone3-5 or with radiotherapy can reduce inflammation-related signs and symptoms in patients with active ophthalmopathy.
- However, glucocorticoids and orbital radiotherapy minimally affect proptosis and can cause dose-limiting adverse reactions.5 In many patients
TEPEZZA
- in patients with Graves’ disease, Immunoglobulins that activate insulin-like growth factor I (IGF-I) receptor (IGF-IR) signaling have been detected
- IGF-I synergistically enhances the actions of thyrotropin IGF-IR is a membraneespanning tyrosine kinase receptor with roles in development and metabolism
- IGF-IR is overexpressed by orbital fibroblasts18 and by T cells and B cells in persons with Graves’ disease.
- (IGF-I) regulates immune function and thus might be targeted therapeutically in autoimmune diseases.
Mechanism of Action
Teprotumumab-trbw’s mechanism of action in patients with Thyroid Eye Disease has not been fully characterized. Teprotumumab-trbw binds to IGF-1R and blocks its activation and signaling.
Schematic
Photographs of Patients that have undergone treatment with Tepezza